Abstract
Background: Umbilical cord blood hematopoietic stem cell transplant (UCBT) has been practiced as an alternative source of hematopoietic stem cells for patients in need of transplantation. Double-units UCBT has been established as a means of achieving a cell dose of at least 2.5x10 7 nucleated cells per kilogram of body weight in adult recipients. The advantages of UCBT include its rapid availability, reduced stringency in terms of human leukocyte antigen (HLA) match requirements, and subsequent increase in access to transplants for racial minorities. Both related and unrelated UCBTs with single or double units have been performed with high rates of success in both pediatric and adult settings to treat a variety of medical conditions.
Prior to undergoing UCBT, recipients must undergo a conditioning regimen to create space in the bone marrow, suppress the immune system to allow for donor stem cell engraftment, and reduce the tumor burden in cases of neoplastic disease. Total body irradiation (TBI) is commonly incorporated into conditioning regimens to enforce these efforts. Although intense myeloablation in general is associated with a lower risk of relapse and graft rejection, greater regimen intensity also leads to a higher rate of transplant related morbidity and mortality (TRM). Inclusion of TBI specifically in conditioning regimens has been shown to result in organ toxicity and subsequent malignant neoplasm. To help mitigate the risks of myeloablative conditioning (MAC) regimens, non-TBI and reduced-intensity conditioning (RIC) regimens have been investigated as a means of reducing TRM and increasing access of transplantation to patients with age disadvantages or significant comorbidities.
Despite ongoing investigation, studies comparing conditioning regimens of UCBT, with and without TBI, remain limited. This study, using real-world data collected from 4 institutions, retrospectively analyzed the impact of TBI as part of MAC or RIC conditioning regimens in patients undergoing UCBT.
Methods: This is a retrospective study that analyzed the outcomes of 136 patients receiving umbilical cord blood transplants at four institutions. Seventy-nine patients received myeloablative condition (MAC), in which 36 underwent TBI and 33 did not; 67 patients received reduced-intensity condition (RIC), in which 24 underwent TBI and 43 did not. Univariate and multivariate analyses were conducted to compare the outcomes and the post-transplant complications between patients who did and did not undergo TBI in MAC subgroup and RIC subgroup, respectively.
Results: Characteristics of UCBT recipients who did and did not undergo TBI, stratified by conditioning regimen were compared with both multivariate and univariate analyses and didn't see significant difference. We didn't observe significant difference in GVHD and transplant-related infection incidence rates between patient subgroup that did and did not undergo TBI as part of their pre-UCBT conditioning regimen via both multivariate and univariate analyses.
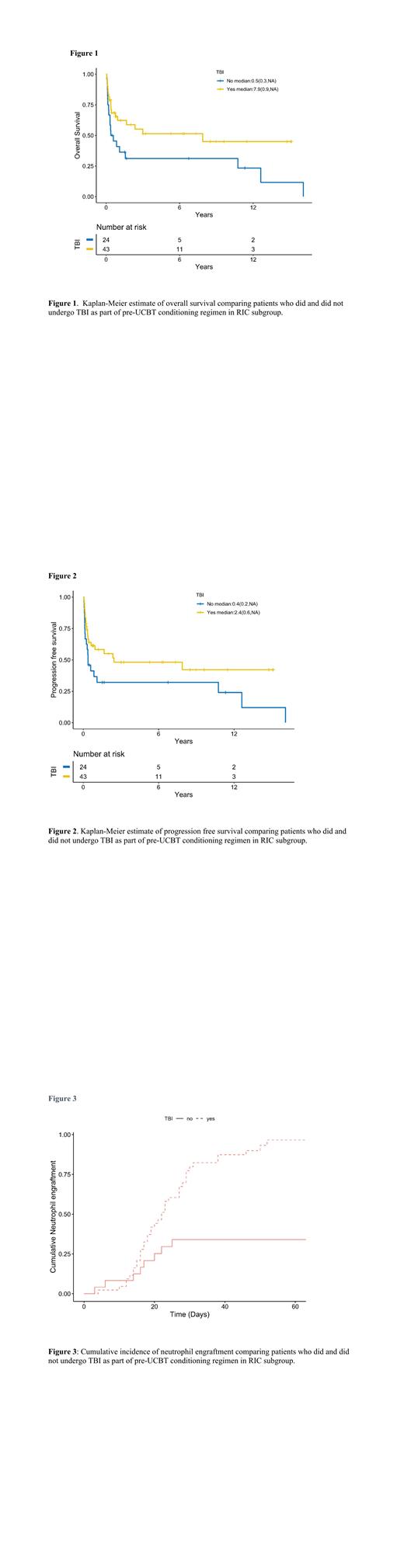
In RIC subgroup, the patients who underwent TBI appeared to have superior overall survival (adjusted hazard ratio [aHR]=0.25, 95% confidence interval [CI]: 0.09-0.66, p=0.005) (Figure 1), progression-free survival (aHR=0.26, 95% CI: 0.10-0.66, p=0.005) (Figure 2), and shorter time to neutrophil engraftment (aHR=6.26, 95% CI: 2.27 - 17.31, p=0.0004) (Figure 3). However, in MAC subgroup, there were no statistically significant difference between using and not using TBI. There were also no differences between the patients who either underwent or not underwent TBI in terms of acute or chronic GVHD rates or rates of transplant-related infections in both subgroups.
Conclusion: Combining with RIC, TBI may improve OS, PFS, and neutrophil engraftment time. However, the incidences of other post-transplant complication were comparable between patients who underwent and did not undergo TBI as part of conditioning regimens during umbilical cord blood transplant.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal